Cardiology Duisburg (NRW): Prof Schöls
Treatment focus
- Cardiac catheter examinations (Diagnosis and treatment of coronary artery disease)
- Catheter-assisted aortic valve replacement (TAVI )
- Catheter-based reconstruction of the mitral valve (MitraClip)
- Atrial septal defects ((ASD), patent foramen ovale (PFO))
- Ventricular septal defect (after myocardial infarction (ischemic ventricular septal defect (VSD))
- Atrial appendage occlusion
Contact
Duisburg Heart Center
Department of Cardiology, Angiology and Electrophysiology
Gerrickstraße 21, D-47137 Duisburg
P: +49 203 3969 3526 F: +49 203 451 3206
Consultation Hours:
Monday-Friday: 7.30 AM - 16.00 PM

Medical Range
Range of Diagnostic Services
Non-Invasive Examination Procedures:
- ECG
- Stress ECG
- Echo
- TEE
- Stress echo
- CT
- MRI
- Stress MRI
Invasive Examination Procedures:
- Cardiac catheterization
- FFR measurement
- IVUS
- OCT
Range of Therapeutic Services
The range of services includes all catheter interventional techniques:
- PTCA
- Stent implantation
- Rotational atherectomy
- Shock wave
- TAVI
- MitraClip
- Tri-clip
- LAA closure
- ASD closure
- PFO closure
- VSD closure
- Foreign object removal
- Temporary circulatory support systems such as Impella and IABP
More Information
Card
Prof Dr Wolfgang Schöls is a specialist in cardiology and head physician of the Department of Cardiology, Angiology, and Electrophysiology at the Duisburg Heart Center of the Evangelisches Klinikum Niederrhein.
Prof Schöls and his team offer heart patients a variety of state-of-the-art procedures with a particular specialization in the gentle, minimally invasive cardiac catheterization technique for the precise diagnosis and treatment of narrowed or occluded coronary arteries, heart valve defects, and other structural heart diseases.
Invasive Cardiology: State-of-the-Art Cardiac Catheter Examinations by Renowned Cardiologists
The discipline of invasive cardiology addresses diagnostic and interventional procedures on the human heart. Corresponding procedures are carried out in the cardiac catheterization laboratory using contrast agents and X-rays not only on the heart and the vessels close to the heart but also on the carotid arteries, the renal arteries, and the peripheral vessels.
Catheters are thin, flexible plastic tubes through which contrast agents can be injected, and balloon catheters can be inserted with or without pre-mounted vascular stents. Access to the heart is obtained through the inguinal or wrist artery against the blood flow.
Thanks to local anesthesia, the vascular puncture is essentially painless; the absence of sensitive nerve fibers inside the vessels and the heart makes general anesthesia unnecessary, and the patient can follow the examination of their heart while awake and talking to the treating physician.
All standard procedures for invasive diagnosis (intravascular flow measurement, intravascular ultrasound, optical coherence tomography) and therapy (balloon dilatation, stenting, rotational atherectomy, shock wave therapy) of constrictions of the coronary vessels are available.
Catheter Assisted Aortic Valve Replacement (TAVI): Gentle Treatment of Aortic Valve Narrowing
Even a healthy lifestyle cannot reliably prevent aortic valve narrowing. The aortic valve acts as a check valve and prevents the backflow of previously ejected blood from the aorta into the left ventricle during the heart's filling phase. If the aortic valve narrows with age, for example, due to calcium deposits, the heart must permanently use enormous forces to pump against the higher resistance.
This can lead to shortness of breath, dizziness, and chest tightness in advanced stages. In such cases, the rigid, inflexible valve should be replaced to restore blood flow and relieve the strain on the heart. Such valve replacement should be performed in an open surgical procedure or by a catheter-based method called TAVI.
This option was initially developed for patients with too high a risk of surgery and anesthesia. TAVI therapy is far less invasive than traditional heart valve surgery. Because the chest is not opened and using a heart-lung machine under anesthesia is not required, the patient can be mobilized from bed on the day of treatment and leave the hospital after a few days of observation.
Because of these advantages, the TAVI procedure is now considered the standard for most patients with aortic valve stenosis. Prof Dr Wolfgang Schöls routinely carries out this treatment as an experienced cardiologist.
Anatomical conditions and concomitant diseases play a decisive role in therapy planning. Detailed preliminary clarification and detailed imaging are therefore essential to propose an optimal therapy for each patient with individual selection of the access route, the type of valve, and the appropriate size.
MitraClip: Interventional Treatment for Mitral Valve Insufficiency
Mitral valve insufficiency refers to leakage of the mitral valve. This is the second most common acquired valvular defect after aortic valve stenosis described above.
If there is a leak in the mitral valve, part of the blood flows back into the left atrium during the heart's action, causing backflow into the pulmonary circulation. Patients experience this as oppressive shortness of breath, suffer from water retention, and have a significant decrease in their ability to cope with everyday life.
If this pathological stress persists over a more extended period, it is accompanied by chronic damage to the heart muscle. Open surgery was the only possible corrective measure for this clinical picture for a long time. Such surgery, however, is not an option for many patients due to severe concomitant diseases, advanced age, or a severe restriction of the heart's pumping function.
Therefore, a catheter-based mitral valve repair procedure using MitraClip has been developed to reduce mitral valve leakage without surgery. A small metal clip is advanced through the inguinal vein to the mitral valve via a controllable catheter. It connects the two leaflets of the mitral valve, allowing the defective valve to close more tightly as a result. Opening of the chest is not required for this procedure.
Experienced Specialist in the Closure of Atrial Septal Defects
Congenital defects ("holes") in the atrial septum are usually detected early and treated by a pediatric cardiologist. In adult patients, the question of catheter-assisted closure rarely arises but is then typically feasible without problems.
The so-called open foramen ovale is far more common, a malformation that can be associated, in particular, with cerebral embolisms. This is a slit-shaped opening in the overlapping area of the two leaves of the atrial septum, which only becomes visible when the pressure in the right atrium exceeds that in the left one.
This connection is essential in the uterus for the unborn child but "grows out of shape" in most cases after birth. The foramen ovale does not close in about 20% of adults; if an open foramen ovale is found in younger patients (< 60 years of age) with a cerebral infarction of unknown cause, then it is presumably important as a portal of passage for blood clots and should be closed.
Such an occlusion can be carried out quite easily via a catheter with a "little umbrella" developed for this purpose. Prof Dr Wolfgang Schöls has been performing these interventions in large numbers for many years, often taking no more than 15 minutes.
Therapy of Acquired Heart Defects: State-of-the-Art Catheter Technology for Ventricular Septal Defects after Heart Attack
Heart muscle tissue dies in the course of a heart attack. This tissue destruction can also affect the cardiac septum. If the dead tissue tears, an ischemic ventricular septal defect develops, a life-threatening complication. The left ventricle pumps only part of the blood into the systemic circulation and the other part through the defect into the right ventricle, which is under pressure.
Surgery is problematic in this situation and carries a high risk. However, such a defect can often be closed early with a catheter-assisted procedure with significantly less risk.
Such a catheter intervention is carried out under sedation, and the positioning of the umbrella is controlled via a swallowing echo probe. Prof Schöls has broad expertise in this relatively rare but life-saving procedure.
Curriculum Vitae
| Since 2018 | Vice Chairman of the Board, German Council for Resuscitation |
| 2006 - 2022 | Medical Director, Duisburg Heart Center |
| Since 2004 | Chief Physician, Clinic for Cardiology and Angiology, Duisburg Heart Center |
| 2000 | Deputy Medical Director of the Department of Internal Medicine III, Heidelberg University Medical Center Head of the Division of Interventional Cardiology Extraordinary Professorship, Medical Faculty of Heidelberg University |
| 1998 | Head of the Electrophysiological Research Group of the Department of Internal Medicine III, Heidelberg University Medical Center |
| 1994 | Habilitation Thesis: "Pathophysiology and Mechanisms of Therapeutic Interventions in Experimental Atrial Fibrillation." |
| 1993 | Appointment as Senior Physician, Department of Internal Medicine III, Heidelberg University Medical Clinic |
| 1990 - 1993 | Research Associate, Department of Internal Medicine III, Heidelberg University Medical Center |
| 1990 | Research Award of the Giessen University Society |
| 1988 - 1990 | Research Fellowship of the German Society of Cardiology and the State University of New York at the Department of Cardiology, State University of New York at Brooklyn, N.Y., USA |
| 1985 - 1988 | Research Assistant, Department of Internal Medicine III, Heidelberg University Medical Center |
| 1982 - 1983 | Thesis: "Electrophysiological Parameters for the Prediction of the Acute Efficacy of Class-Ic Antiarrhythmic Agents in the Awake Dog." |
| 1979 - 1985 | Medical Studies at the University of Heidelberg |
Team
- Dr Ute Ruprecht
- Senior Physician in Charge / Head of Section Electrophysiology
- Dr Ilse Janicke
Senior Physician in Charge - Dr Mathias Kullmer
Senior Physician in Charge Cardiac Catheter Lab
Plus, another 12 senior physicians and 27 assistant physicians
Extras
Interdisciplinary care of diseases in the overlapping areas is possible due to the close interaction with the Departments of Cardiac Surgery and the Department of Pediatric Cardiology and Adults with Congenital Heart Defects. This applies to combined interventional and cardiac surgery (hybrid interventions). The immediate spatial coexistence of cardiac surgery and cardiology and the immediate availability of cardiac surgery expertise increases the safety of interventional procedures.
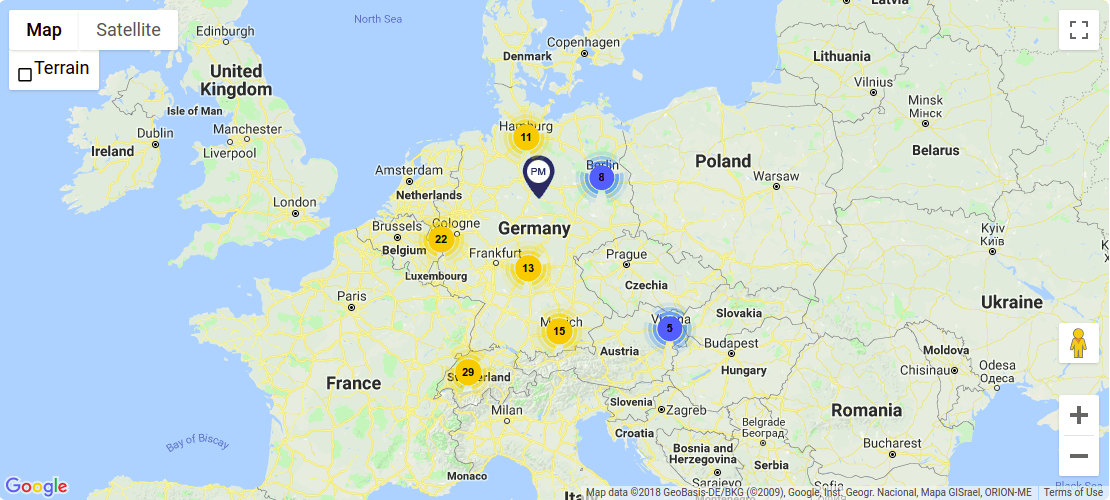
Transport Connections
| Duisburg Main Station | 6.6 km |
| Essen/Mühlheim Airport | 21 km |
| Düsseldorf Airport | 28 km |
| Cologne/Bonn Airport | 75 km |
Information about Duisburg
Duisburg is the hinge into three regions: the idyllic Lower Rhine, the bubbling Ruhr area, and the legendary Rhine rail.
Duisburg, the inland port city on the Rhine and Ruhr, stretches from the western edge of the Ruhr metropolis to the Lower Rhine and merges with the Rhine rail to the south. The city sees itself as a hub of tourist and logistical routes and assumes an interesting hinge function within the varied regions.